♦ What is tuberculosis (TB)?
Tuberculosis (TB), also known colloquially as the "white death", or historically as consumption, is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria.
Tuberculosis generally affects the lungs, but it can also affect other parts of the body.
Most infections show no symptoms, in which case it is known as latent tuberculosis.
Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected.
Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss.
Infection of other organs can cause a wide range of symptoms.
Tuberculosis is spread from one person to the next through the air when people who have active TB in their lungs cough, spit, speak, or sneeze.
People with latent TB do not spread the disease.
Active infection occurs more often in people with HIV/AIDS and in those who smoke.
Diagnosis of Active TB is based on chest X-rays, as well as microscopic examination and culture of body fluids.
Diagnosis of Latent TB relies on the tuberculin skin test (TST) or blood tests.
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and vaccination with the bacillus Calmette-Guérin (BCG) vaccine.
Those at high risk include household, workplace, and social contacts of people with active TB.
Treatment requires the use of multiple antibiotics over a long period of time.
Antibiotic resistance is a growing problem, with increasing rates of multiple drug-resistant tuberculosis (MDR-TB).
In 2018, one quarter of the world's population was thought to have a latent infection of TB.
New infections occur in about 1% of the population each year.
In 2022, an estimated 10.6 million people developed active TB, resulting in 1.3 million deaths, making it the second leading cause of death from an infectious disease after COVID-19.
Tuberculosis has been present in humans since ancient times.
♦ History
Tuberculosis has existed since antiquity.
The oldest unambiguously detected M. tuberculosis gives evidence of the disease in the remains of bison in Wyoming dated to around 17.000 years ago.
However, whether tuberculosis originated in bovines, then transferred to humans, or whether both bovine and human tuberculosis diverged from a common ancestor, remains unclear.
A comparison of the genes of M. tuberculosis complex (MTBC) in humans to MTBC in animals suggests humans did not acquire MTBC from animals during animal domestication, as researchers previously believed. Both strains of the tuberculosis bacteria share a common ancestor, which could have infected humans even before the Neolithic Revolution.
Skeletal remains show some prehistoric humans (4000 BC) had TB, and researchers have found tubercular decay in the spines of Egyptian mummies dating from 3000 to 2400 BC.
Before the Industrial Revolution, folklore often associated tuberculosis with vampires.
When one member of a family died from the disease, the other infected members would lose their health slowly. People believed this was caused by the original person with TB draining the life from the other family members.
- Identification
Robert Koch identified and described the bacillus causing tuberculosis, M. tuberculosis, on 24 March 1882. In 1905, he was awarded the Nobel Prize in Physiology or Medicine for this discovery.
Robert Koch did not believe the cattle and human tuberculosis diseases were similar, which delayed the recognition of infected milk as a source of infection. During the first half of the 1900s, the risk of transmission from this source was dramatically reduced after the application of the pasteurization process. Koch announced a glycerine extract of the tubercle bacilli as a "remedy" for tuberculosis in 1890, calling it "tuberculin".
Although it was not effective, it was later successfully adapted as a screening test for the presence of pre-symptomatic tuberculosis.
- Development of treatments
In Europe, rates of tuberculosis began to rise in the early 1600s to a peak level in the 1800s, when it caused nearly 25% of all deaths.
In the 18th and 19th century, tuberculosis had become epidemic in Europe, showing a seasonal pattern.
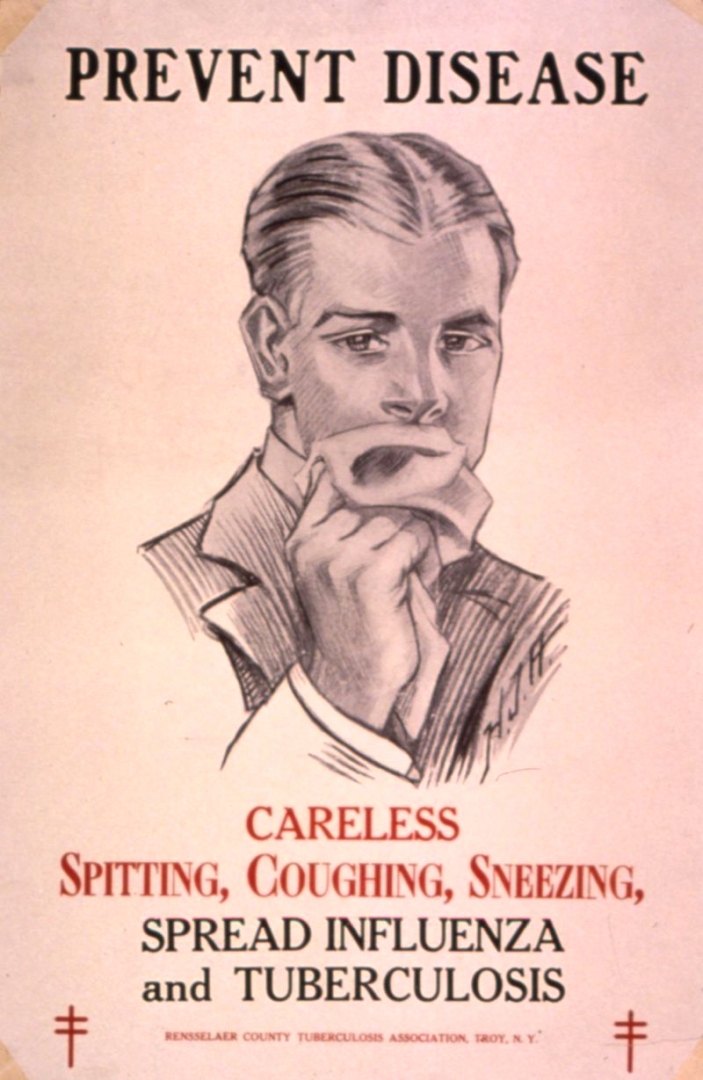
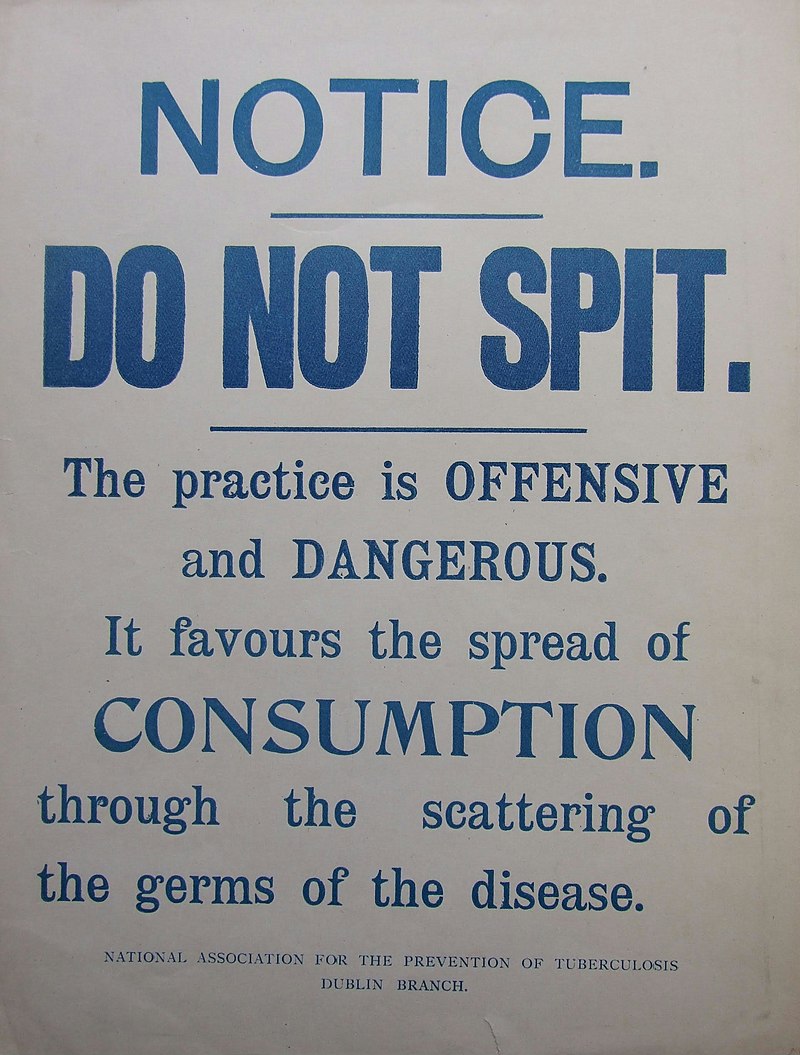
Tuberculosis caused widespread public concern in the 19th and early 20th centuries as the disease became common among the urban poor.
In 1815, one in four deaths in England was due to "consumption".
By 1918, TB still caused one in six deaths in France.
After TB was determined to be contagious, in the 1880s, it was put on a notifiable-disease list in Britain; campaigns started to stop people from spitting in public places, and the infected poor were "encouraged" to enter sanatoria that resembled prisons (the sanatoria for the middle and upper classes offered excellent care and constant medical attention).
Whatever the benefits of the "fresh air" and labor in the sanatoria, even under the best conditions, 50% of those who entered died within five years (c. 1916).
Albert Calmette and Camille Guérin achieved the first genuine success in immunization against tuberculosis in 1906, using attenuated bovine-strain tuberculosis.
It was called bacille Calmette–Guérin (BCG).
The BCG vaccine was first used on humans in 1921 in France, but achieved widespread acceptance in the US, Great Britain, and Germany only after World War II
By the 1950s mortality in Europe had decreased about 90%.
Improvements in sanitation, vaccination, and other public-health measures began significantly reducing rates of tuberculosis even before the arrival of streptomycin and other antibiotics, although the disease remained a significant threat.
In 1946, the development of the antibiotic streptomycin made effective treatment and cure of TB a reality. Prior to the introduction of this medication, the only treatment was surgical intervention, including the "pneumothorax technique", which involved collapsing an infected lung to "rest" it and to allow tuberculous lesions to heal
- Current reemergence
Because of the emergence of multidrug-resistant tuberculosis (MDR-TB), surgery has been re-introduced for certain cases of TB infections.
It involves the removal of infected chest cavities ("bullae") in the lungs to reduce the number of bacteria and to increase exposure of the remaining bacteria to antibiotics in the bloodstream.
Hopes of eliminating TB ended with the rise of drug-resistant strains in the 1980s.
The subsequent resurgence of tuberculosis resulted in the declaration of a global health emergency by the World Health Organization (WHO) in 1993.
♦ Signs and symptoms
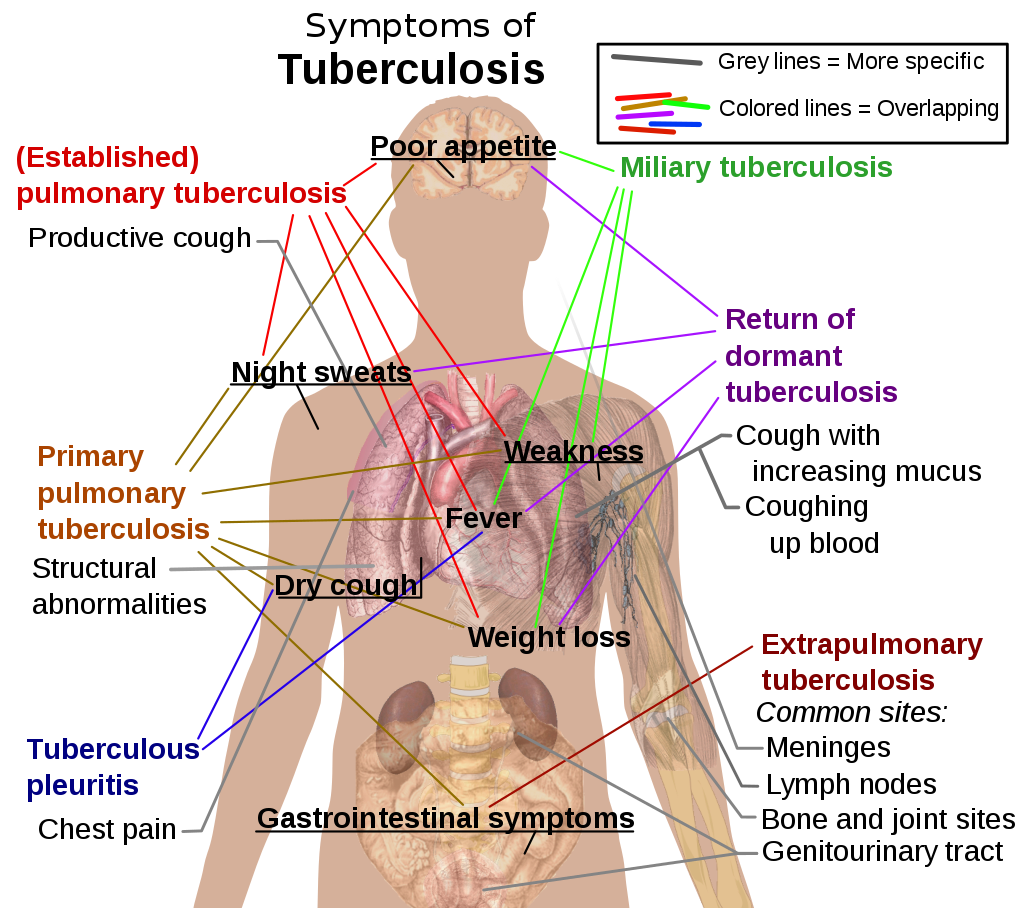
The main symptoms of variants and stages of tuberculosis are given, with many symptoms overlapping with other variants, while others are more (but not entirely) specific for certain variants.
Multiple variants may be present simultaneously.
Tuberculosis may infect any part of the body, but most commonly occurs in the lungs (known as pulmonary tuberculosis).
Extrapulmonary TB occurs when tuberculosis develops outside of the lungs, although extrapulmonary TB may coexist with pulmonary TB.
General signs and symptoms include fever, chills, night sweats, loss of appetite, weight loss, and fatigue.
Significant nail clubbing may also occur.
- Pulmonary
If a tuberculosis infection does become active, it most commonly involves the lungs (in about 90% of cases).
Symptoms may include chest pain and a prolonged cough producing sputum.
About 25% of people may not have any symptoms (i.e., they remain asymptomatic).
Occasionally, people may cough up blood in small amounts, and in very rare cases, the infection may erode into the pulmonary artery or a Rasmussen's aneurysm, resulting in massive bleeding.
Tuberculosis may become a chronic illness and cause extensive scarring in the upper lobes of the lungs. The upper lung lobes are more frequently affected by tuberculosis than the lower ones.
The reason for this difference is not clear.
It may be due to either better air flow, or poor lymph drainage within the upper lungs.
- Extrapulmonary
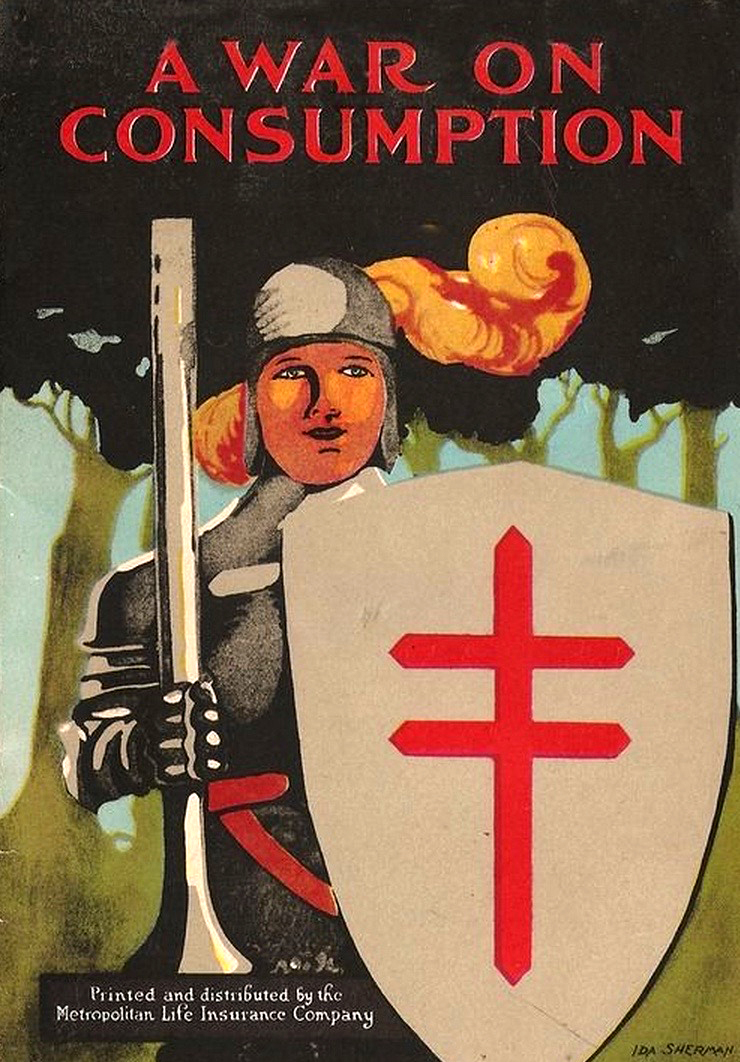
In 15–20% of active cases, the infection spreads outside the lungs, causing other kinds of TB.
These are collectively denoted as extrapulmonary tuberculosis.
Extrapulmonary TB occurs more commonly in people with a weakened immune system and young children.
In those with HIV, this occurs in more than 50% of cases.
Notable extrapulmonary infection sites include the pleura (in tuberculous pleurisy), the central nervous system (in tuberculous meningitis), the lymphatic system (in scrofula of the neck), the genitourinary system (in urogenital tuberculosis), and the bones and joints (in Pott disease of the spine), among others.
A potentially more serious, widespread form of TB is called "disseminated tuberculosis"; it is also known as miliary tuberculosis.
Miliary TB currently makes up about 10% of extrapulmonary cases.
♦ Causes
- Mycobacteria
The main cause of TB is Mycobacterium tuberculosis (MTB), a small, aerobic, nonmotile bacillus.
The high lipid content of this pathogen accounts for many of its unique clinical characteristics.
It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour.
Mycobacteria have an outer membrane lipid bilayer.
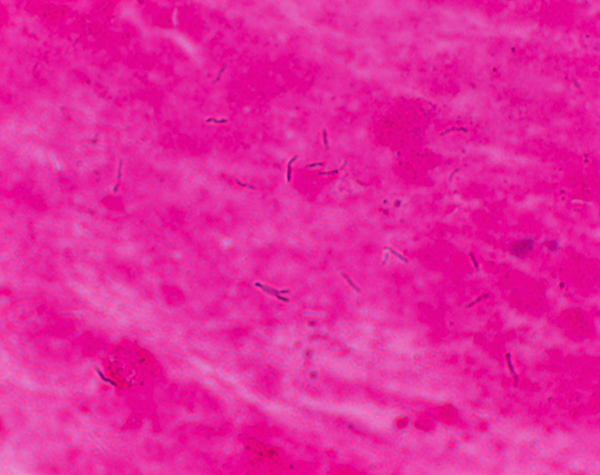
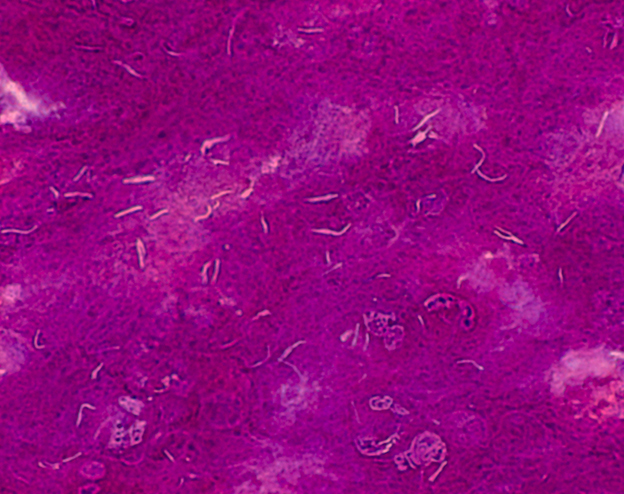
If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and mycolic acid content of its cell wall.
MTB can withstand weak disinfectants and survive in a dry state for weeks.
In nature, the bacterium can grow only within the cells of a host organism, but M. tuberculosis can be cultured in the laboratory.
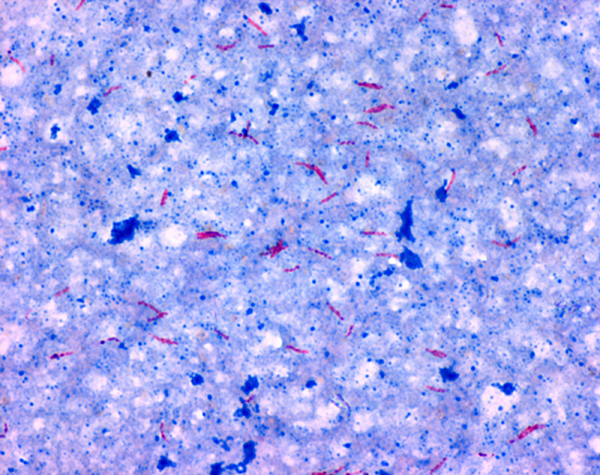
Since MTB retains certain stains even after being treated with acidic solution, it is classified as an acid-fast bacillus.
The most common acid-fast staining techniques are the Ziehl–Neelsen stain and the Kinyoun stain, which dye acid-fast bacilli a bright red that stands out against a blue background.
Auramine-rhodamine staining and fluorescence microscopy are also used.
The M. tuberculosis complex (MTBC) includes four other TB-causing mycobacteria:
M. bovis, M. africanum, M. canettii, and M. microti.
M. africanum is not widespread, but it is a significant cause of tuberculosis in parts of Africa.
M. bovis was once a common cause of tuberculosis, but the introduction of pasteurized milk has almost eliminated this as a public health problem in developed countries.
M. canettii is rare and seems to be limited to the Horn of Africa, although a few cases have been seen in African emigrants.
M. microti is also rare and is seen almost only in immunodeficient people, although its prevalence may be significantly underestimated.
Other known pathogenic mycobacteria include M. leprae, M. avium, and M. kansasii.
The latter two species are classified as "nontuberculous mycobacteria" (NTM) or atypical mycobacteria. NTM cause neither TB nor leprosy, but they do cause lung diseases that resemble TB.
- Transmisson
When people with active pulmonary TB cough, sneeze, speak, sing, or spit, they expel infectious aerosol droplets 0.5 to 5.0 µm in diameter.
A single sneeze can release up to 40,000 droplets. Each one of these droplets may transmit the disease, since the infectious dose of tuberculosis is very small (the inhalation of fewer than 10 bacteria may cause an infection).
- Risk of transmission
People with prolonged, frequent, or close contact with people with TB are at particularly high risk of becoming infected, with an estimated 22% infection rate.
A person with active but untreated tuberculosis may infect 10–15 (or more) other people per year.
Transmission should occur from only people with active TB – those with latent infection are not thought to be contagious.
If someone become infected, it typically takes three to four weeks before the newly infected person becomes infectious enough to transmit the disease to others.
♦ Pathogenesis
About 90% of those infected with M. tuberculosis have asymptomatic, latent TB infections (sometimes called LTBI), with only a 10% lifetime chance that the latent infection will progress to overt, active tuberculous disease.
In those with HIV, the risk of developing active TB increases to nearly 10% a year.
If effective treatment is not given, the death rate for active TB cases is up to 66%.
TB infection begins when the mycobacteria reach the alveolar air sacs of the lungs, where they invade and replicate within endosomes of alveolar macrophages.
Macrophages identify the bacterium as foreign and attempt to eliminate it by phagocytosis.
During this process, the bacterium is enveloped by the macrophage and stored temporarily in a membrane-bound vesicle called a phagosome. The phagosome then combines with a lysosome to create a phagolysosome. In the phagolysosome, the cell attempts to use reactive oxygen species and acid to kill the bacterium.
However, M. tuberculosis has a thick, waxy mycolic acid capsule that protects it from these toxic substances.
M. tuberculosis is able to reproduce inside the macrophage and will eventually kill the immune cell.
The primary site of infection in the lungs, known as the Ghon focus, is generally located in either the upper part of the lower lobe, or the lower part of the upper lobe.
Tuberculosis of the lungs may also occur via infection from the blood stream. This is known as a Simon focus and is typically found in the top of the lung.
This hematogenous transmission can also spread infection to more distant sites, such as peripheral lymph nodes, the kidneys, the brain, and the bones.
All parts of the body can be affected by the disease, though for unknown reasons it rarely affects the heart, skeletal muscles, pancreas, or thyroid.
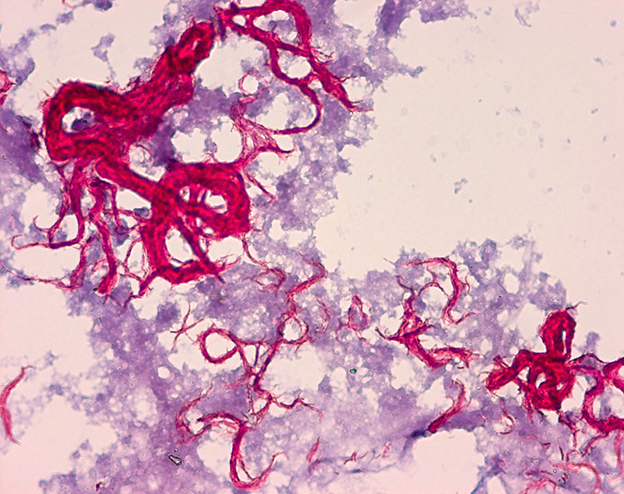
Tuberculosis is classified as one of the granulomatous inflammatory diseases.
Macrophages, epithelioid cells, T lymphocytes, B lymphocytes, and fibroblasts aggregate to form granulomas, with lymphocytes surrounding the infected macrophages.
When other macrophages attack the infected macrophage, they fuse together to form a giant multinucleated cell in the alveolar lumen. The granuloma may prevent dissemination of the mycobacteria and provide a local environment for interaction of cells of the immune system.
However, more recent evidence suggests that the bacteria use the granulomas to avoid destruction by the host's immune system. Macrophages and dendritic cells in the granulomas are unable to present antigen to lymphocytes; thus the immune response is suppressed.
Bacteria inside the granuloma can become dormant, resulting in latent infection.
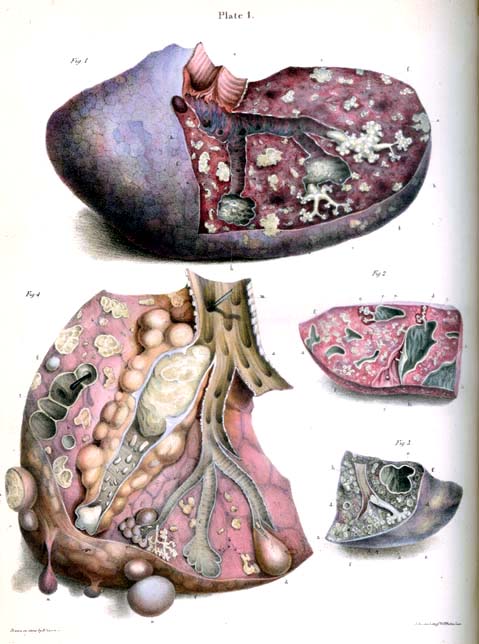
Another feature of the granulomas is the development of abnormal cell death (necrosis) in the center of tubercles.
To the naked eye, this has the texture of soft, white cheese and is termed caseous necrosis.
- miliary tuberculosis
If TB bacteria gain entry to the blood stream from an area of damaged tissue, they can spread throughout the body and set up many foci of infection, all appearing as tiny, white tubercles in the tissues.
This severe form of TB disease, most common in young children and those with HIV, is called miliary tuberculosis.
People with this disseminated TB have a high fatality rate even with treatment (about 30%).
♦ Diagnosis
- Active tuberculosis
Diagnosing active tuberculosis based only on signs and symptoms is difficult, as is diagnosing the disease in those who have a weakened immune system.
A diagnosis of TB should, however, be considered in those with signs of lung disease or constitutional symptoms lasting longer than two weeks.
A chest X-ray and multiple sputum cultures for acid-fast bacilli are typically part of the initial evaluation.
Interferon-γ release assays (IGRA) and tuberculin skin tests are of little use in most of the developing world.
A definitive diagnosis of TB is made by identifying M. tuberculosis in a clinical sample (e.g., sputum, pus, or a tissue biopsy). However, the difficult culture process for this slow-growing organism can take two to six weeks for blood or sputum culture.
Thus, treatment is often begun before cultures are confirmed.
Nucleic acid amplification tests and adenosine deaminase testing may allow rapid diagnosis of TB.
Blood tests to detect antibodies are not specific or sensitive, so they are not recommended.
- Latent tuberculosis
The Mantoux tuberculin skin test is often used to screen people at high risk for TB.
Those who have been previously immunized with the Bacille Calmette-Guerin vaccine may have a false-positive test result.
The test may be falsely negative in those with sarcoidosis, Hodgkin's lymphoma, malnutrition, and most notably, active tuberculosis.
♦ Prevention
Tuberculosis prevention and control efforts rely primarily on the vaccination of infants and the detection and appropriate treatment of active cases.
- Vaccines
The only available vaccine as of 2021 is bacillus Calmette-Guérin (BCG).
In children it decreases the risk of getting the infection by 20% and the risk of infection turning into active disease by nearly 60%.
It is the most widely used vaccine worldwide, with more than 90% of all children being vaccinated.
The immunity it induces decreases after about ten years.
♦ Prognosis
Progression from TB infection to overt TB disease occurs when the bacilli overcome the immune system defenses and begin to multiply.
In primary TB disease (some 1–5% of cases), this occurs soon after the initial infection.
However, in the majority of cases, a latent infection occurs with no obvious symptoms.
These dormant bacilli produce active tuberculosis in 5–10% of these latent cases, often many years after infection.
The risk of reactivation increases with immunosuppression, such as that caused by infection with HIV.
In people coinfected with M. tuberculosis and HIV, the risk of reactivation increases to 10% per year.
The chance of death from a case of tuberculosis is about 4% as of 2008, down from 8% in 1995.
In people with smear-positive pulmonary TB (without HIV co-infection), after 5 years without treatment, 50-60% die while 20-25% achieve spontaneous resolution (cure). TB is almost always fatal in those with untreated HIV co-infection and death rates are increased even with antiretroviral treatment of HIV.
♦ Epidemiology
Roughly one-quarter of the world's population has been infected with M. tuberculosis, with new infections occurring in about 1% of the population each year.
However, most infections with M. tuberculosis do not cause disease, and 90–95% of infections remain asymptomatic.
In 2012, an estimated 8.6 million chronic cases were active.
In 2010, 8.8 million new cases of tuberculosis were diagnosed, and 1.20–1.45 million deaths occurred (most of these occurring in developing countries).
Of these, about 0.35 million occur in those also infected with HIV.
In 2018, tuberculosis was the leading cause of death worldwide from a single infectious agent.
The total number of tuberculosis cases has been decreasing since 2005, while new cases have decreased since 2002.
♦ Society and culture
- Names
Tuberculosis has been known by many names from the technical to the familiar.
Phthisis (Φθισις) is a Greek word for consumption, an old term for pulmonary tuberculosis; around 460 BCE, Hippocrates described phthisis as a disease of dry seasons.
The abbreviation TB is short for tubercle bacillus.
Consumption was the most common nineteenth century English word for the disease, and was also in use well into the twentieth century.
- Art and literature
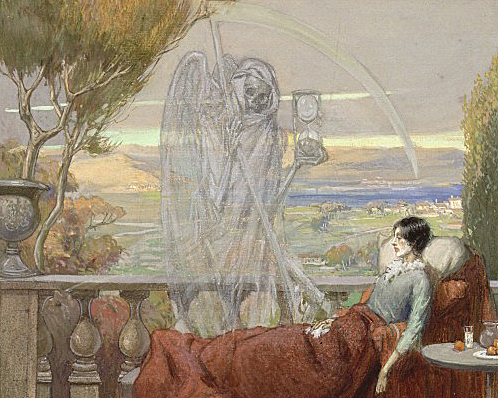
Tuberculosis was for centuries associated with poetic and artistic qualities among those infected, and was also known as "the romantic disease".
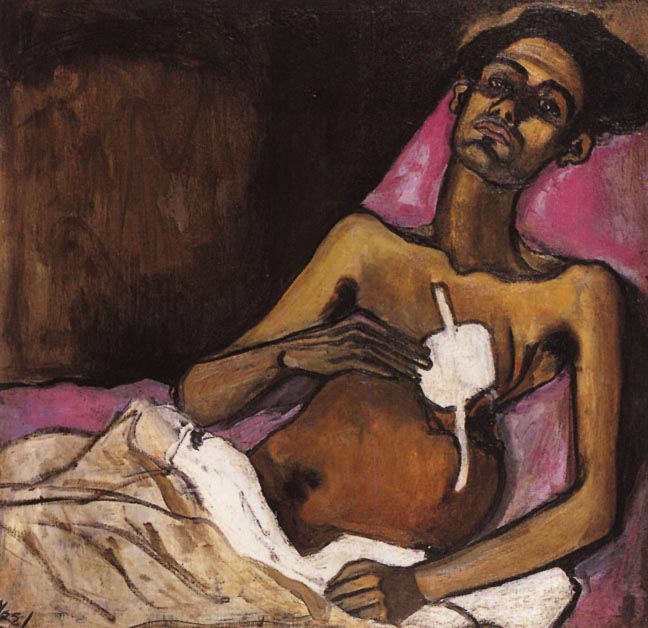
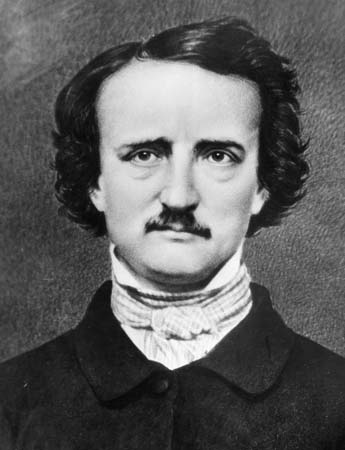
Major artistic figures such as the poets John Keats, Percy Bysshe Shelley, and Edgar Allan Poe, the composer Frédéric Chopin, the playwright Anton Chekhov, the novelists Franz Kafka, Katherine Mansfield, Charlotte Brontë, Fyodor Dostoevsky, Thomas Mann, W. Somerset Maugham, George Orwell, and Robert Louis Stevenson, and the artists Alice Neel, Jean-Antoine Watteau, Elizabeth Siddal, Marie Bashkirtseff, Edvard Munch, Aubrey Beardsley and Amedeo Modigliani either had the disease or were surrounded by people who did.
A widespread belief was that tuberculosis assisted artistic talent. Physical mechanisms proposed for this effect included the slight fever and toxaemia that it caused, allegedly helping them to see life more clearly and to act decisively.
Tuberculosis formed an often-reused theme in literature, as in Thomas Mann's The Magic Mountain, set in a sanatorium; in music, as in Van Morrison's song "T.B. Sheets"; in opera, as in Puccini's La bohème and Verdi's La Traviata; in art, as in Monet's painting of his first wife Camille on her deathbed; and in film, such as the 1945 The Bells of St. Mary's starring Ingrid Bergman as a nun with tuberculosis.
Tuberculosis (TB)
Related
References
https://en.wikipedia.org/wiki/Tuberculosis
Photos
wikipedia
large photo tuberculosis: B. Erkernap
MMIZ, ErasmusMC, Rotterdam_Loes van Damme
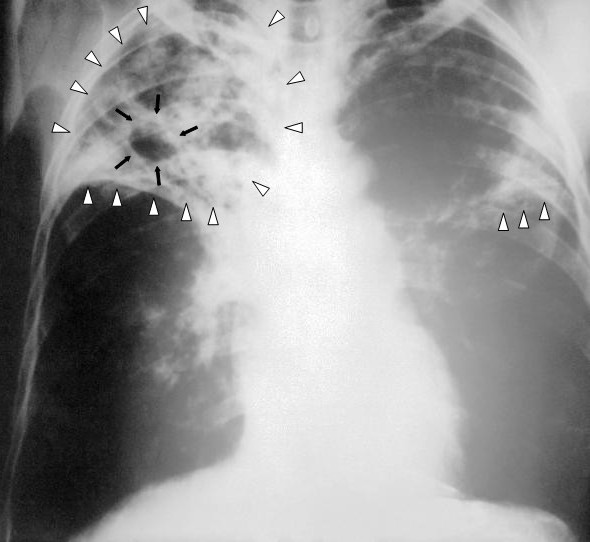
Chest X-ray of a person with advanced tuberculosis: Infection in both lungs is marked by white arrow-heads, and the formation of a cavity is marked by black arrows
- Actinomycosis
- Anthrax
- Biopsy Sinusitis_Aspergillus flavus
- Botulism
- Brucellosis
- Cat Scratch Disease
- Cellulitis
- Cholera
- Creutzfeldt-Jakob Disease
- Cystic Fibrosis_CF
- Diphtheria
- Erysipelas
- Erysipeloid or fish poison
- Legionnaires disease
- Lemierre syndrome
- Leprosy
- Listeriosis
- Lyme / Borreliosis
- Melioidosis
- Meningitis
- Plague
- Syphilis
- Tetanus
- Trench Mouth_Plaut-Vincent_acute necrotizing ulcerative gingivitis
- Tuberculosis (TB)
- Tularemia_Rabbit Fever
- Typhoid fever (Epidemic typhus)
- Whooping Cough