♦ What is leprosy?
Leprosy, also known as Hansen's disease (HD), is a long-term infection by the bacteria Mycobacterium leprae.
Infection can lead to damage of the nerves, respiratory tract, skin, and eyes. This nerve damage may result in a lack of ability to feel pain, which can lead to the loss of parts of a person's extremities from repeated injuries or infection through unnoticed wounds.
An infected person may also experience muscle weakness and poor eyesight.
Leprosy symptoms may begin within one year, but, for some people, symptoms may take 20 years or more to occur.
♦ Spread
Leprosy is spread between people, although extensive contact is necessary.
Leprosy has a low pathogenicity, and 95% of people who contract M. leprae do not develop the disease.
Spread is thought to occur through a cough or contact with fluid from the nose of a person infected by leprosy.
Genetic factors and immune function play a role in how easily a person catches the disease.
Leprosy occurs more commonly among people living in poverty.
Leprosy does not spread during pregnancy to the unborn child or through sexual contact.
♦ Two types
There are two main types of the disease
- paucibacillary
- multibacillary,
which differ in the number of bacteria present.
A person with paucibacillary disease has five or fewer poorly pigmented, numb skin patches, while a person with multibacillary disease has more than five skin patches.
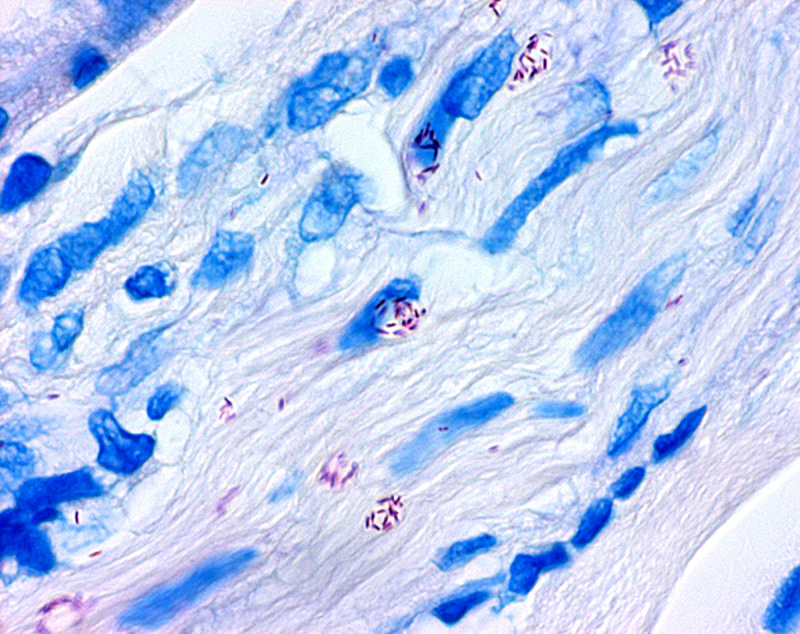
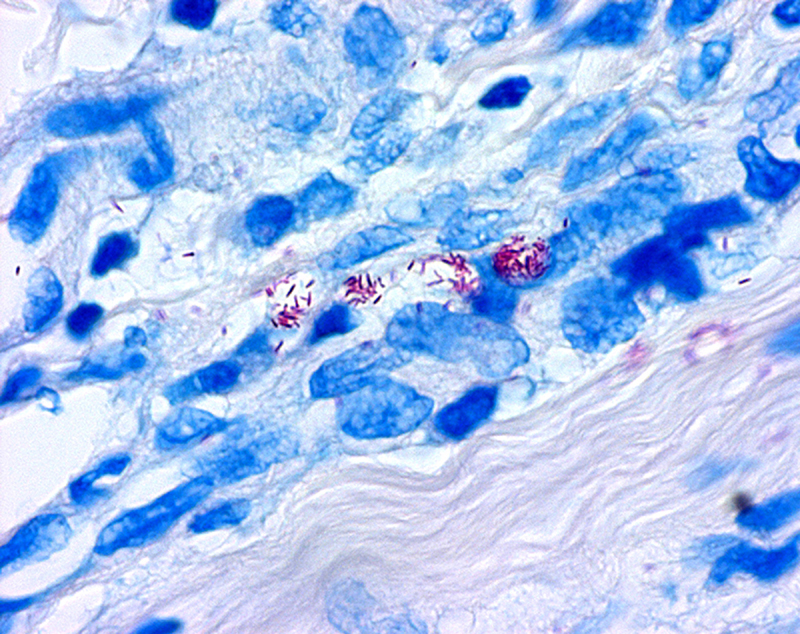
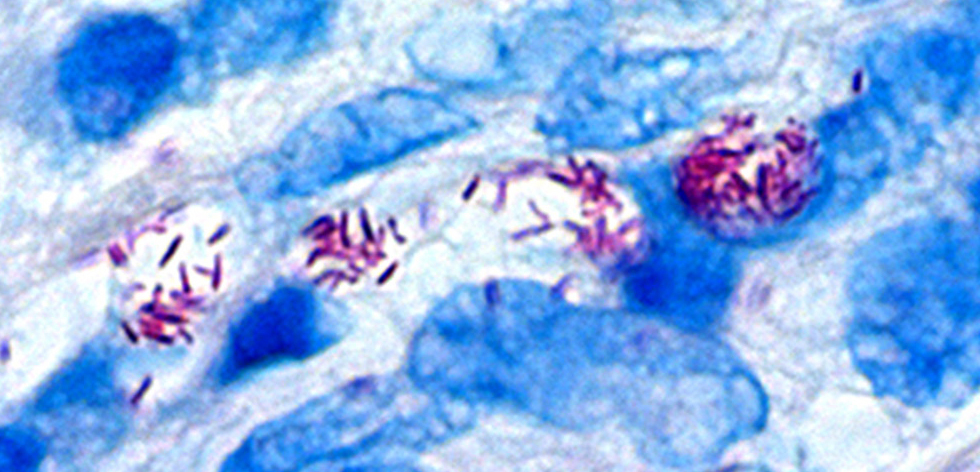
The diagnosis is confirmed by finding acid-fast bacilli in a biopsy of the skin.
♦ Treatment
Leprosy is curable with multidrug therapy.
Treatment of paucibacillary leprosy is with the medications dapsone, rifampicin, and clofazimine for six months.
Treatment for multibacillary leprosy uses the same medications for 12 months.
A number of other antibiotics may also be used.
These treatments are provided free of charge by the World Health Organization.
♦ Contagious
Leprosy is not highly contagious.
People with leprosy can live with their families and go to school and work.
In the 1980s, there were 5.2 million cases globally, but by 2020 this decreased to fewer than 200,000.
Most new cases occur in 14 countries, with India accounting for more than half.
In the 20 years from 1994 to 2014, 16 million people worldwide were cured of leprosy.
About 200 cases per year are reported in the United States. Central Florida accounted for 81% of cases in Florida and nearly 1 out of 5 leprosy cases nationwide.
Separating people affected by leprosy by placing them in leper colonies still occurs in some areas of India, China, the African continent, and Thailand.
Leprosy has affected humanity for thousands of years.
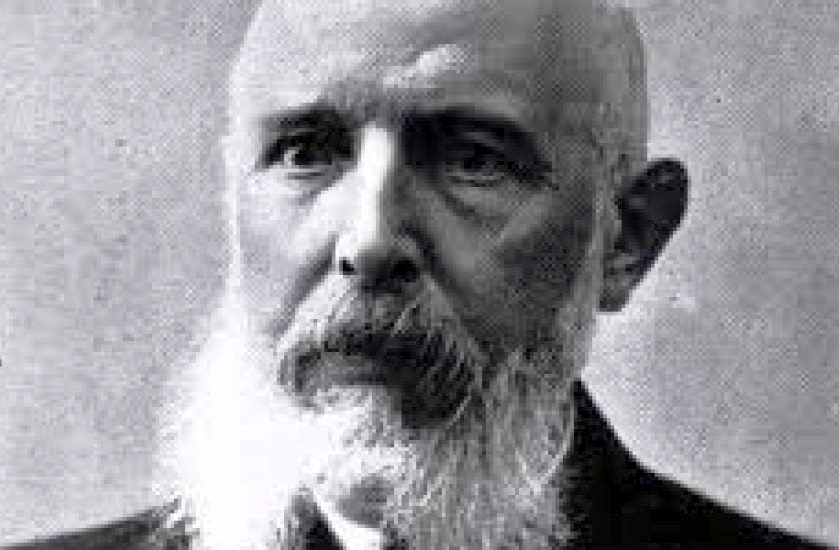
The disease takes its name from the Greek word λέπρᾱ (léprā), from λεπῐ́ς (lepís; 'scale'), while the term "Hansen's disease" is named after the Norwegian physician Gerhard Armauer Hansen.
♦ Social stigma
Leprosy has historically been associated with social stigma, which continues to be a barrier to self-reporting and early treatment.
Some consider the word leper offensive, preferring the phrase "person affected with leprosy".
Leprosy is classified as a neglected tropical disease.
World Leprosy Day was started in 1954 to draw awareness to those affected by leprosy.
♦ Signs and symptoms
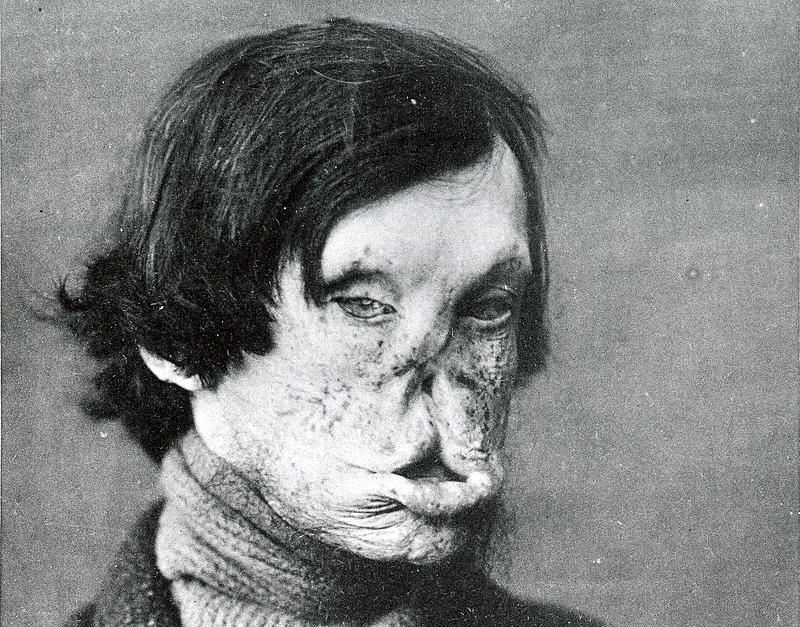
Common symptoms present in the different types of leprosy include a runny nose; dry scalp; eye problems; skin lesions; muscle weakness; reddish skin; smooth, shiny, diffuse thickening of facial skin, ear, and hand; loss of sensation in fingers and toes; thickening of peripheral nerves; a flat nose from destruction of nasal cartilages; and changes in phonation and other aspects of speech production.
In addition, atrophy of the testes and impotence may occur.
Leprosy can affect people in different ways.
♦ Incubation time
The average incubation period is five years.
People may begin to notice symptoms within the first year or up to 20 years after infection.
The first noticeable sign of leprosy is often the development of pale or pink coloured patches of skin that may be insensitive to temperature or pain.
Patches of discolored skin are sometimes accompanied or preceded by nerve problems including numbness or tenderness in the hands or feet.
Secondary infections (additional bacterial or viral infections) can result in tissue loss, causing fingers and toes to become shortened and deformed, as cartilage is absorbed into the body. A person's immune response differs depending on the form of leprosy.
Approximately 30% of people affected with leprosy experience nerve damage.
The nerve damage sustained is reversible when treated early, but becomes permanent when appropriate treatment is delayed by several months.
Damage to nerves may cause loss of muscle function, leading to paralysis. It may also lead to sensation abnormalities or numbness, which may lead to additional infections, ulcerations, and joint deformities.
♦ Cause
M. leprae and M. lepromatosis are the mycobacteria that cause leprosy.
M. lepromatosis is a relatively newly identified mycobacterium isolated from a fatal case of diffuse lepromatous leprosy in 2008.
M. lepromatosis is indistinguishable clinically from M. leprae.
M. leprae is an intracellular, acid-fast bacterium that is aerobic and rod-shaped.
M. leprae is surrounded by the waxy cell envelope coating characteristic of the genus Mycobacterium.
Genetically, M. leprae and M. lepromatosis lack the genes that are necessary for independent growth.
M. leprae and M. lepromatosis are obligate intracellular pathogens, and cannot be grown (cultured) in the laboratory.
While the causative organisms have to date been impossible to culture in vitro, it has been possible to grow them in animals such as mice and armadillos.
Multilocus sequence typing of the armadillo M. leprae strains suggests that they were of human origin for at most a few hundred years. Thus, it is suspected that armadillos first acquired the organism incidentally from early American explorers.
This incidental transmission was sustained in the armadillo population, and it may be transmitted back to humans, making leprosy a zoonotic disease (spread between humans and animals).
♦ Risk factors
The greatest risk factor for developing leprosy is contact with another person infected by leprosy.
People who are exposed to a person who has leprosy are 5-8 times more likely to develop leprosy than members of the general population.
Leprosy also occurs more commonly among those living in poverty.
Not all people who are infected with M. leprae develop symptoms.
Conditions that reduce immune function, such as malnutrition, other illnesses, or genetic mutations, may increase the risk of developing leprosy.
Infection with HIV does not appear to increase the risk of developing leprosy.
♦ Transmission
Transmission of leprosy occurs during close contact with those who are infected.
Transmission of leprosy is through the upper respiratory tract.
Older research suggested the skin as the main route of transmission, but research has increasingly favored the respiratory route.
Transmission occurs through inhalation of bacilli present in upper airway secretion.
Leprosy is not sexually transmitted and is not spread through pregnancy to the unborn child.
The majority (95%) of people who are exposed to M. leprae do not develop leprosy; casual contact such as shaking hands and sitting next to someone with leprosy does not lead to transmission.
People are considered non-infectious 72 hours after starting appropriate multi-drug therapy.
♦ Diagnosis
Testing for loss of sensation with monofilament
In countries where people are frequently infected, a person is considered to have leprosy if they have one of the following two signs:
- Skin lesion consistent with leprosy and with definite sensory loss
- Positive skin smears
Skin lesions can be single or many, and usually hypopigmented, although occasionally reddish or copper-colored. The lesions may be flat (macules), raised (papules), or solid elevated areas (nodular).
Experiencing sensory loss at the skin lesion is a feature that can help determine if the lesion is caused by leprosy or by another disorder such as tinea versicolor.
Thickened nerves are associated with leprosy and can be accompanied by loss of sensation or muscle weakness, but muscle weakness without the characteristic skin lesion and sensory loss is not considered a reliable sign of leprosy.
n some cases, acid-fast leprosy bacilli in skin smears are considered diagnostic; however, the diagnosis is typically made without laboratory tests, based on symptoms. If a person has a new leprosy diagnosis and already has a visible disability caused by leprosy, the diagnosis is considered late.
In countries or areas where leprosy is uncommon, such as the United States, diagnosis of leprosy is often delayed because healthcare providers are unaware of leprosy and its symptoms. Early diagnosis and treatment prevent nerve involvement, the hallmark of leprosy, and the disability it causes.
There is no recommended test to diagnose latent leprosy in people without symptoms.
Few people with latent leprosy test positive for anti PGL-1. The presence of M. leprae bacterial DNA can be identified using a polymerase chain reaction (PCR)-based technique.
This molecular test alone is not sufficient to diagnose a person, but this approach may be used to identify someone who is at high risk of developing or transmitting leprosy such as those with few lesions or an atypical clinical presentation.
♦ Complications
Leprosy may cause the victim to lose limbs and digits but not directly. M. leprae attacks nerve endings and destroys the body's ability to feel pain and injury.
Without feeling pain, people with leprosy have an increased risk of injuring themselves. Injuries become infected and result in tissue loss. Fingers, toes, and limbs become shortened and deformed as the tissue is absorbed into the body.
♦ Prevention
Early detection of the disease is important, since physical and neurological damage may be irreversible even if cured.
Medications can decrease the risk of those living with people who have leprosy from acquiring the disease and likely those with whom people with leprosy come into contact outside the home.
The WHO recommends that preventive medicine be given to people who are in close contact with someone who has leprosy.
The suggested preventive treatment is a single dose of rifampicin (SDR) in adults and children over 2 years old who do not already have leprosy or tuberculosis. Preventive treatment is associated with a 57% reduction in infections within 2 years and a 30% reduction in infections within 6 years.
♦ Vaccin
The Bacillus Calmette–Guérin (BCG) vaccine offers a variable amount of protection against leprosy in addition to its closely related target of tuberculosis. It appears to be 26% to 41% effective (based on controlled trials) and about 60% effective based on observational studies with two doses possibly working better than one.
The WHO concluded in 2018 that the BCG vaccine at birth reduces leprosy risk and is recommended in countries with high incidence of TB and people who have leprosy. People living in the same home as a person with leprosy are suggested to take a BCG booster which may improve their immunity by 56%. Development of a more effective vaccine is ongoing.
A novel vaccine called LepVax entered clinical trials in 2017 with the first encouraging results reported on 24 participants published in 2020. If successful, this would be the first leprosy-specific vaccine available.
♦ Outcomes
Although leprosy has been curable since the mid-20th century, left untreated it can cause permanent physical impairments and damage to a person's nerves, skin, eyes, and limbs.
Despite leprosy not being very infectious and having a low pathogenicity, there is still significant stigma and prejudice associated with the disease. Because of this stigma, leprosy can affect a person's participation in social activities and may also affect the lives of their family and friends.
People with leprosy are also at a higher risk for problems with their mental well-being.
The social stigma may contribute to problems obtaining employment, financial difficulties, and social isolation.
Efforts to reduce discrimination and reduce the stigma surrounding leprosy may help improve outcomes for people with leprosy.
Leprosy
Related
References
https://en.wikipedia.org/wiki/Leprosy
Photos
MMIZ, ErasmusMC, Rotterdam_Loes van Damme
wikipedia
https://en.wikipedia.org/wiki/Gerhard_Armauer_Hansen
https://en.wikiversity.org/wiki/WikiJournal_Preprints/Leprosy

- Actinomycosis
- Anthrax
- Biopsy Sinusitis_Aspergillus flavus
- Botulism
- Brucellosis
- Cat Scratch Disease
- Cellulitis
- Cholera
- Creutzfeldt-Jakob Disease
- Cystic Fibrosis_CF
- Diphtheria
- Erysipelas
- Erysipeloid or fish poison
- Legionnaires disease
- Lemierre syndrome
- Leprosy
- Listeriosis
- Lyme / Borreliosis
- Melioidosis
- Meningitis
- Plague
- Syphilis
- Tetanus
- Trench Mouth_Plaut-Vincent_acute necrotizing ulcerative gingivitis
- Tuberculosis (TB)
- Tularemia_Rabbit Fever
- Typhoid fever (Epidemic typhus)
- Whooping Cough