♦ What is diphtheria?
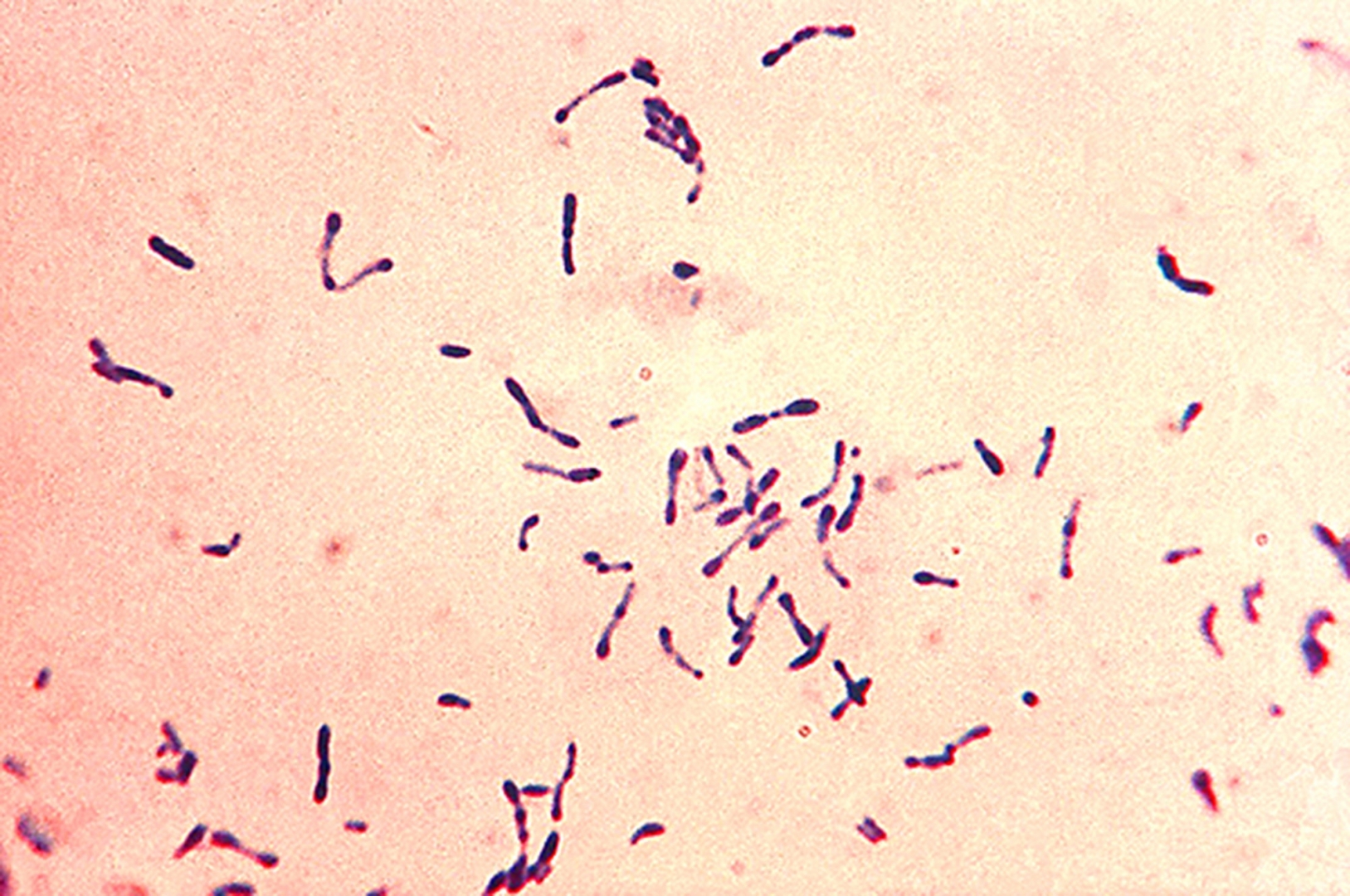
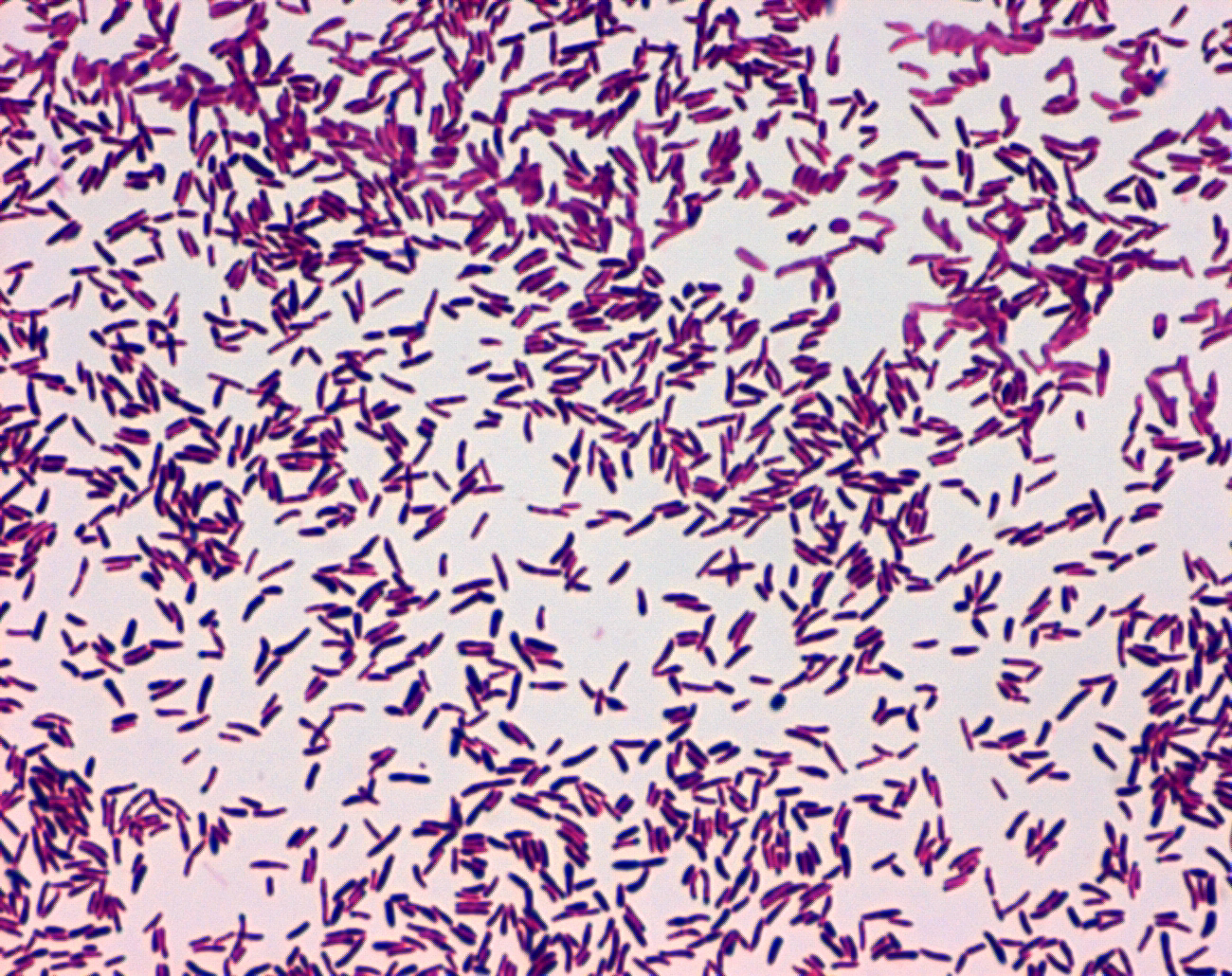
Is an infection caused by the bacterium Corynebacterium diphtheriae.
♦ Signs and symptoms
The symptoms of diphtheria usually begin two to seven days after infection.
Symptoms of diphtheria include fever of 38 °C (100.4 °F) or above, chills, fatigue, bluish skin coloration (cyanosis), sore throat, hoarseness, cough, headache, difficulty swallowing, painful swallowing, difficulty breathing, rapid breathing, foul-smelling and bloodstained nasal discharge, and lymphadenopathy.
Within two to three days, diphtheria may destroy healthy tissues in the respiratory system. The dead tissue forms a thick, gray coating that can build up in the throat or nose. This thick gray coating is called a “pseudomembrane.” It can cover tissues in the nose, tonsils, voice box, and throat, making it very hard to breathe and swallow.
Symptoms can also include cardiac arrhythmias, myocarditis, and cranial and peripheral nerve palsies.
♦ Diphtheritic croup
Laryngeal diphtheria can lead to a characteristic swollen neck and throat, or "bull neck". The swollen throat is often accompanied by a serious respiratory condition, characterized by a brassy or "barking" cough, stridor, hoarseness, and difficulty breathing, and historically referred to variously as "diphtheritic croup", "true croup", or sometimes simply as "croup".
Diphtheritic croup is extremely rare in countries where diphtheria vaccination is customary. As a result, the term "croup" nowadays most often refers to an unrelated viral illness that produces similar but milder respiratory symptoms.
♦ Transmission
Human-to-human transmission of diphtheria typically occurs through the air when an infected individual coughs or sneezes. Breathing in particles released from the infected individual leads to infection.
Contact with any lesions on the skin can also lead to transmission of diphtheria, but this is uncommon.
Indirect infections can occur, as well. If an infected individual touches a surface or object, the bacteria can be left behind and remain viable.
♦ Diagnosis
The current clinical case definition of diphtheria used by the United States' Centers for Disease Control and Prevention is based on both laboratory and clinical criteria.
• Laboratory criteria
- Isolation of C. diphtheriae from a Gram stain or throat culture from a clinical specimen
- Histopathologic diagnosis of diphtheria by Albert's stain
• Clinical criteria
- Upper respiratory tract illness with sore throat
- Low-grade fever (above 39 °C (102 °F) is rare)
- An adherent, dense, grey pseudomembrane covering the posterior aspect of the pharynx: in severe cases, it can extend to cover the entire tracheobronchial tree.
• Case classification
- Probable: a clinically compatible case that is not laboratory-confirmed and is not epidemiologically linked to a laboratory-confirmed case
- Confirmed: a clinically compatible case that is either laboratory-confirmed or epidemiologically linked to a laboratory-confirmed case
Empirical treatment should generally be started in a patient in whom suspicion of diphtheria is high.
♦ Vaccination
A diphtheria vaccine is effective for prevention and available in a number of formulations.
Three or four doses, given along with tetanus vaccine and pertussis vaccine, are recommended during childhood. Further doses of diphtheria-tetanus vaccine are recommended every ten years.
Protection can be verified by measuring the antitoxin level in the blood.
Previous infection may not protect against future infection.
♦ Treatment
Diphtheria can be treated with the antibiotics erythromycin or benzylpenicillin. These antibiotics may also be used for prevention in those who have been exposed to the infection.
A tracheotomy is sometimes needed to open the airway in severe cases.
♦ Epidemiology
Diphtheria is fatal in between 5% and 10% of cases. In children under five years and adults over 40 years, the fatality rate may be as much as 20%.
In 2013, it resulted in 3,300 deaths, down from 8,000 deaths in 1990.
The number of cases has changed over the course of the last 2 decades, specifically throughout developing countries. Better standards of living, mass immunization, improved diagnosis, prompt treatment, and more effective health care have led to the decrease in cases worldwide. However, although outbreaks are rare, they still occur worldwide, especially in developed nations such as Germany among unvaccinated children.
In Nazi Germany contagious diseases such as diphtheria were among the leading causes of morbidity; they increased “after the mid-1920s, doubled again between 1932 and 1937, and reached extremely high levels during the war only to decline rapidly thereafter”.
After the breakup of the former Soviet Union in the early 1990s, vaccination rates in its constituent countries fell so low that an explosion of diphtheria cases occurred. In 1991, 2,000 cases of diphtheria occurred in the USSR. Between 1991 and 1998 as many as 200,000 cases in the Commonwealth of Independent States were reported, with 5,000 deaths.
♦ History
- In 1613, Spain experienced an epidemic of diphtheria. The year is known as El Año de los Garrotillos (The Year of Strangulations) in the history of Spain.
- In 1735, a diphtheria epidemic swept through New England.
- Before 1826, diphtheria was known by different names across the world.
- In England, it was known as Boulogne sore throat, as it spread from France. In 1826, Pierre Bretonneau gave the disease the name diphthérite (from Greek diphthera "leather") describing the appearance of pseudomembrane in the throat.
- In 1856, Victor Fourgeaud described an epidemic of diphtheria in California.
- In 1878, Queen Victoria's daughter Princess Alice and her family became infected with diphtheria, causing two deaths, Princess Marie of Hesse and by Rhine and Princess Alice herself.
- In 1883, Edwin Klebs identified the bacterium causing diphtheria and named it Klebs-Loeffler bacterium. The club shape of this bacterium helped Edwin to differentiate it from other bacteria. Over the period of time, it was called Microsporon diphtheriticum, Bacillus diphtheriae, and Mycobacterium diphtheriae.
Current nomenclature is Corynebacterium diphtheriae.
- Friedrich Loeffler was the first person to cultivate C. diphtheriae in 1884. He used Koch's postulates to prove association between C. diphtheriae and diphtheria. He also showed that the bacillus produces an exotoxin.
Diphtheria
Related
References
https://en.wikipedia.org/wiki/Diphtheria
Photos
wiki media
MMIZ, ErasmusMC, Rotterdam_Loes van Damme

- Actinomycosis
- Anthrax
- Biopsy Sinusitis_Aspergillus flavus
- Botulism
- Brucellosis
- Cat Scratch Disease
- Cellulitis
- Cholera
- Creutzfeldt-Jakob Disease
- Cystic Fibrosis_CF
- Diphtheria
- Erysipelas
- Erysipeloid or fish poison
- Legionnaires disease
- Lemierre syndrome
- Leprosy
- Listeriosis
- Lyme / Borreliosis
- Melioidosis
- Meningitis
- Plague
- Syphilis
- Tetanus
- Trench Mouth_Plaut-Vincent_acute necrotizing ulcerative gingivitis
- Tuberculosis (TB)
- Tularemia_Rabbit Fever
- Typhoid fever (Epidemic typhus)
- Whooping Cough