Brucella melitensis
-
General information
Brucella cultures should be handled using BSL-3 practices, with culture manipulations being done in a biological safety cabinet.
General information
Brucella from Sir David Bruce (1855-1931), microbiologist in Australia and England.
Brucellosis continues to be one of the most common laboratory-acquired infections.
Practices associated with transmission in the laboratory include unprotecting handling of specimens, sniffing of plates, mouth pipetting and exposure of the eyes, nose, or mouth to infectious aerosols.
Taxonomy
Family: Brucellaceae
Natural habitats
Brucella are facultative intracellular parasites, taking as their natural habitat a variety of animal species.
Human pathogen in order of decreasing virulence
B. melitensis - Malta fever sheep, goats, alpacas and camel
B. suis - Brucellosis pigs, swine, reindeer and caribou
B. abortus - Bang's disease cattle, camels, buffalo, yaks and horses
B. canis - Brucellosis dogs
Malditof knows only B. melitensis
Clinical significance
Transmission from human to human is very rare
Brucellosis
Although the disease can begin acutely, the beginning is usually insidious and is characterized by slight fever without local symptoms.
The fever is irregular and is accompanied with complaints of headache, malaise, fatigue, sweating and joint problems.
They can live intracellular and invade a variety of tissues.
Incubation period of 1 week to 2-3 months.
Sometimes it proceeds acutely with wavy fever (febris undulans).
They spread into the bloodstream and localize in the liver, spleen, bone and other tissues and form granulomas there.
Are therefore difficult to reach for the immune system and antibiotics.
Complications include bacterial endocarditis, nephritis, meningoencephalitis and orchitis.
The fatality rate is <1% and is mainly associated with the occurrence of bacterial endocarditis.
In non-zoonotic areas the infection proceeds possibly exacerbated by doctor's delay, probably due to a slower running diagnostics because the disease is low in the differential diagnosis.
Serology
Usually the diagnosis is established by serological testing.
Practical nature of the reasons are: it can take up to 4 weeks before a culture is positive and in practice, the patient is often already used antibiotics, so the culture is useless.
-
Diseases
-
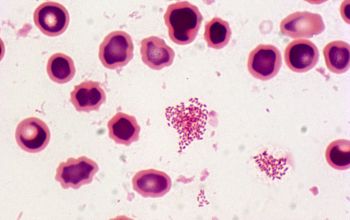
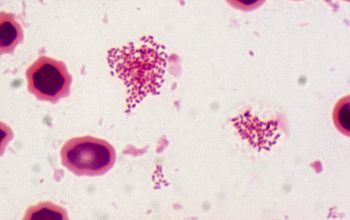
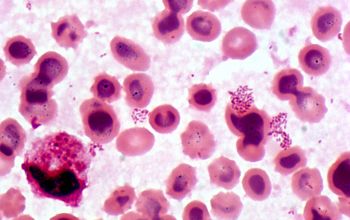
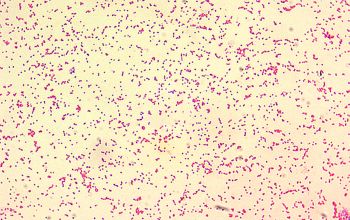
Gram stain
Very small Gram negative coccobacillus,
0.5-0.7 x 0.6-1.5 µm,
They do not usually show bipolar staining
they appear predominately single or in groups.
Brucella is the smallest Gram-negative organism (except F. tularensis)
-
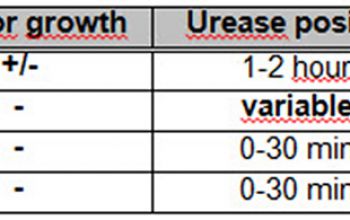
Culture characteristics
-
Culture is considered the "gold standard" in the laboratory diagnosis of brucellosis.
Obligate aerobic,
5-10% CO2 improves the growth
BA: grows after about 1 to 3 (4-5) days, as a very small, round, smooth glittering and translucent, without hemolysis or pigment.
Brucella may change from smooth to rough colonies, this is based on the composition of the LPS (lipopolysaccharide) from the cell wall.
However smooth colonies are more resistant to killing by the leuco’s than the rough LPS.
McConkey: no growth (variable)
BBAØ: no growth
Blood Culture Bottles
The blood culture bottles hold 14days.
Most Brucella species are within 7 days of incubation were found using the BACTEC, some take longer.
-
-
Characteristics
-
References
James Versalovic et al.(2011) Manual of Clinical Microbiology 10th Edition
Karen C. Carrol et al (2019) Manual of Clinical Microbiology, 12th Edition